Residents in Maine’s prisons are finding substance use disorder recovery and rehabilitation. But a record number of Mainers outside the prison walls are dying alone in bedrooms, bathrooms and alleyways, despite the state’s massive, multifaceted outreach initiatives.
Maine’s overdose death rate remains one of the highest in the nation, according to the Centers for Disease Control. Illegal drug overdoses killed 716 people last year, three times more Mainers than a decade ago.
The state’s success in treating those in prisons is leaving government officials and those in the recovery community searching for ways to bring the model to the general public.
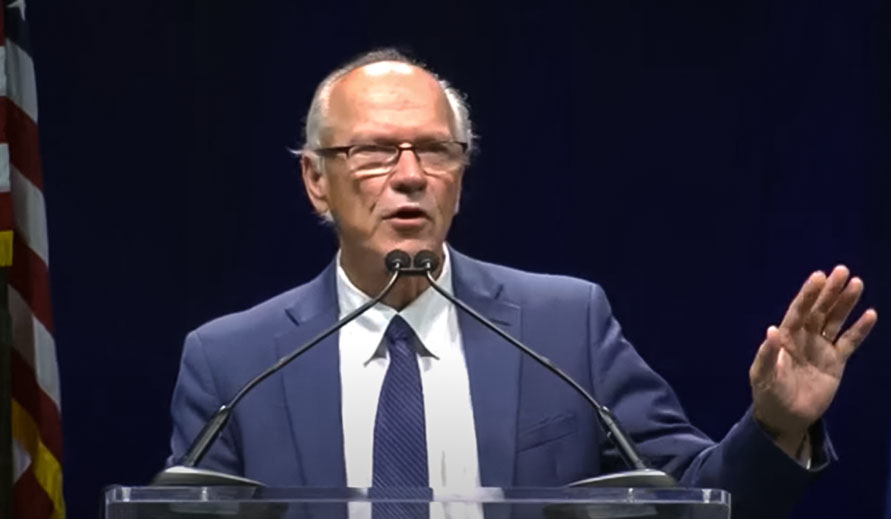
“We won’t save every single person, but we should not be losing 700 people a year in this state,” said Maine’s Director of Opioid Response Gordon Smith. “We can do better and we will do better.”
Of the state’s 10,000 overdoses, about 7 percent were fatal last year. Maine’s overdose death rate, 47.1 deaths per 100,000 people, is nearly double California’s at 26.6 per 100,000 people, according to the Centers for Disease Control.
Without immediate intervention after an overdose, even more could die, Smith said.
The Department of Corrections model substance use disorder program of recovery is working in its controlled environment, drastically improving the climate inside the state’s six facilities, according to DOC officials.
Success is harder to come by outside the prisons with two major Mexican cartels pushing more deadly drugs into the well-known drug trafficking route running up the I-95 corridor from Florida to Maine, according to Smith.
The last exit on I-95 is in Houlton.
Newest on the scene is the deadly animal tranquilizer, xylazine, which naloxone cannot reverse. Currently, 80 percent of the state’s drug fatalities are tied to fentanyl, which is 100 times more potent than morphine. Even methamphetamine is blended with fentanyl, Smith said.
“We have to keep pace with what we are seeing in the drug supply. It is very, very lethal right now and that’s why we are losing as many people as we do,” Smith said. Many times those with substance use disorder are not even aware that fentanyl is in the drugs they are using, he said.

The stigma associated with substance use can make treatment elusive for many because stigma leads to shame and shame kills people, said Penny Guisinger, recovery programs director for Healthy Acadia.
When people feel shame they use alone perhaps in an upstairs bedroom or bathroom while the people downstairs may not even know, Smith said. If no one checks on them until the next morning, it’s too late, he said.
A lack of affordable housing options plays a role in overdose deaths. About 10 percent who died from a drug overdose last year did not have homes, Smith said.
“We can’t expect people who don’t know where they are going to sleep tonight to be really focused on their own recovery,” he said. “There’s a continuum. People need help with detox, residential care, recovery residence, recovery friendly workplaces and support through their lifetime.”
With such grim numbers, it’s hard to see that change is happening. The state has made huge leaps in putting the pieces in place for prevention and recovery to happen under Gov. Janet Mills’ administration.
More than 1,300 recovery coaches are trained. Hundreds of thousands of doses of naloxone are distributed. Opioid pain prescriptions are cut in half. The Department of Corrections has one of the most progressive opioid responses in the nation. The Legislature passed a harm reduction law in June. Millions of dollars are allocated to treatment and prevention programs. A total of $235 million in opioid settlement funds will be distributed over 18 years. The state’s OPTIONS liaisons in every county follow up on non-fatal overdoses to offer options.
And all counties, with the exception of Aroostook, have treatment courts in place.
“The changes I’ve seen, since I started doing this work in 2017, to catch us up to other states, have been amazing,” said Denise Black, co-director of the Maine Alliance for Recovery Coaching, Healthy Acadia. “When we started there were no recovery coaches around here at all and now people are hiring recovery coaches. We’ve shifted tremendously. Our state partners have been such advocates of this work.”
Aroostook County, with seven overdose deaths in May alone, has trailed the state’s other counties in recovery and prevention resources. But that too is changing, according to Smith.
Aroostook has two recovery centers, two residential recovery centers, a methadone clinic and a jail that has one of the highest percentages of its residents on medication for substance use disorder, he said.
More residential beds are moving from Limestone to Presque Isle. The city is also slated for detox beds and within the next eight to 12 months, from 100 to 200 additional beds will be available in The County, Smith said.
A work group meets regularly with Aroostook County District Attorney Todd Collins to make sure all the pieces are in place to get a treatment court up and running in 2024.
Senate President Troy Jackson, who sponsored the drug court legislation, said the original bill may need to be amended in the next session, but he is pleased with the progress thus far.
The successful Department of Corrections pilot program kicked off in 2019 at Maine Correctional Center in Windham. It provides methadone, suboxone or sublocade for residents with substance use disorder and six months left on their sentences, said Department of Corrections Deputy Commissioner Anthony Cantillo.
The department now offers the program to all residents in state correctional facilities, regardless of the time remaining on their sentences.
About 61 percent of the resident population at the state’s six correctional facilities have an active substance use disorder and 49 percent have an active opiate use disorder, he said.
The correction department’s nationally recognized success goes beyond medication, Cantillo said. It changed philosophy, focusing on removing stigma and humanizing interactions with residents. The current approach is restorative and less adversarial, he said.
Residents also have extensive educational and work-related opportunities, access to a laptop, an open internet platform and job training.
Recovery coaches also work with correctional facility residents via Zoom and help get them connected to a recovery community and resources, if that’s what they want, when they are released, Black said.
“I think their approach, prevention, treatment, harm reduction, overdose prevention all working together and continuing to move toward success is the way,” Black said. “Just like recovery is an ongoing process, so is the answer.”
Recovery coaches are in every county, Black said, adding that Healthy Acadia’s recovery coach services are free and funded by the Maine Office of Behavioral Health.
“The loss of lives is tragic, but at the same time the beauty of recovery is happening. I think that’s the best kept secret. People are finding recovery,” she said.







